The Black Side Of Synthetic Data For Medical Sector.

The use of synthetic data in the medical sector has been gaining traction in recent years. Synthetic data is artificially generated data that can be used in place of real data for research purposes. It has been touted as a solution to some of the challenges faced by medical researchers, such as privacy concerns and limited access to real patient data. However, there is a growing concern about the potential negative consequences of using synthetic data in the medical sector.
In this article, we will explore the black side of synthetic data for medical research. We will delve into what synthetic data is and why it is being used in the medical sector. We will also examine the potential benefits and ethical concerns surrounding the use of synthetic data. Furthermore, we will discuss the limitations of synthetic data in medical research and provide case studies of the negative consequences of using synthetic data. Finally, we will emphasize the importance of data collection and human data validation in the medical sector.
What Is Synthetic Data And Why Is It Being Used In The Medical Sector?
Synthetic data is becoming increasingly popular in the medical sector as a solution to improving machine learning and deep learning model accuracy. This approach is also used to increase training dataset size while staying compliant with data privacy regulations, and enabling predictions of rare diseases. Synthetic data can be applied for various purposes in healthcare, such as simulation and prediction research, hypothesis testing, epidemiology/public health research, health IT development, education and training, public release of datasets, and linking data.
The use of synthetic data can help resolve the issue of accessing sensitive medical information for training algorithms without adding bureaucratic burdens to obtain it. It employs approaches intended to maintain specific statistical properties from the original data source. However, the question surrounding its ethical considerations regarding potential trade-offs and risks should be explored before application.

Moreover, synthetic data has its limitations when creating fake patient records or medical images that do not identify individuals. In light of this limitation in accurately representing real-world experiences within the context of clinical trials or population-based studies using artificial populations rather than those from actual patients may have drawbacks. Hence there is a need to regulate this approach's adoption fully so that potential malicious activities are kept at bay while also facilitating safe access by researchers who could benefit significantly from them.
The Potential Benefits Of Synthetic Data For Medical Research
Synthetic data is an emerging technology that has gained a lot of attention in the medical research field. The use of synthetic data in medical research can minimize the need for personal data while improving machine learning and deep learning model accuracy. The main advantage of synthetic data is that it does not expose sensitive or confidential information to any party, making it ideal for privacy-concerned industries like finance and healthcare.
Moreover, rare diseases are often difficult to study because there may not be enough suitable patients to draw conclusions from. Synthetic data can help to overcome this challenge by generating vast amounts of virtual patient data which could reflect realistic patients suffering from different rare conditions. This creates new potential areas for researchers who need access to large datasets with many variables.
However, it's essential to note that the quality of synthetic data relies on the quality of input data and level of privacy protection used in its creation. As a result, rigorous testing is necessary before using synthetic models in real-world scenarios. Despite the challenges ahead, we expect to see more explorations into the innovative power behind synthetic data's use within medical research as technology rapidly progresses.
The Ethical Concerns Surrounding The Use Of Synthetic Data In Medical Research
Synthetic data, which is created artificially for building algorithms, is set to overtake real data in the medical sector by 2030. Financial investments into synthetic data are increasing rapidly, but there are potential benefits and risks involved in its use.
In medical research, synthetic data can be used for simulation and prediction research, epidemiology/public health research, health IT development, education and training, public release of datasets, and linking data. It can help researchers refine their queries and build provisional models while keeping sensitive patient data safe in Trusted Research Environments. However, the lack of availability of patient data to the broader ML research community has been a significant challenge.
The use of synthetic data raises concerns about vulnerabilities in software and challenges to current policy. For-profit companies acquiring vast healthcare system databases poses new challenges to the protection of patients' privacy. Additionally, there are ethical considerations when using synthetic data for research analysis and statistics. Commonly perceived risks include limited knowledge of patients due to lack of evidence for accuracy of tests or efficacy of treatments and potential misuse of the information by insurance providers or employers.

As such ethical review is essential when embarking on this kind of project involving humans as subjects. Any raised issues should be addressed so that successful outcomes can be achieved without compromising on ethical practices while making sure all parties benefit from sound decisions around big-data initiatives that could generate remarkable payoffs along with huge pitfalls if not correctly handled.
The Limitations Of Synthetic Data In Medical Research
Synthetic data has emerged as a viable solution to protect sensitive patient information in the healthcare industry. However, there are several limitations to its use in medical research. Validating synthetic data requires comparison with original data, which is challenging due to privacy concerns that limit access to patient data. There are limited validation studies on synthetic health data for primary uses with clinical implications.
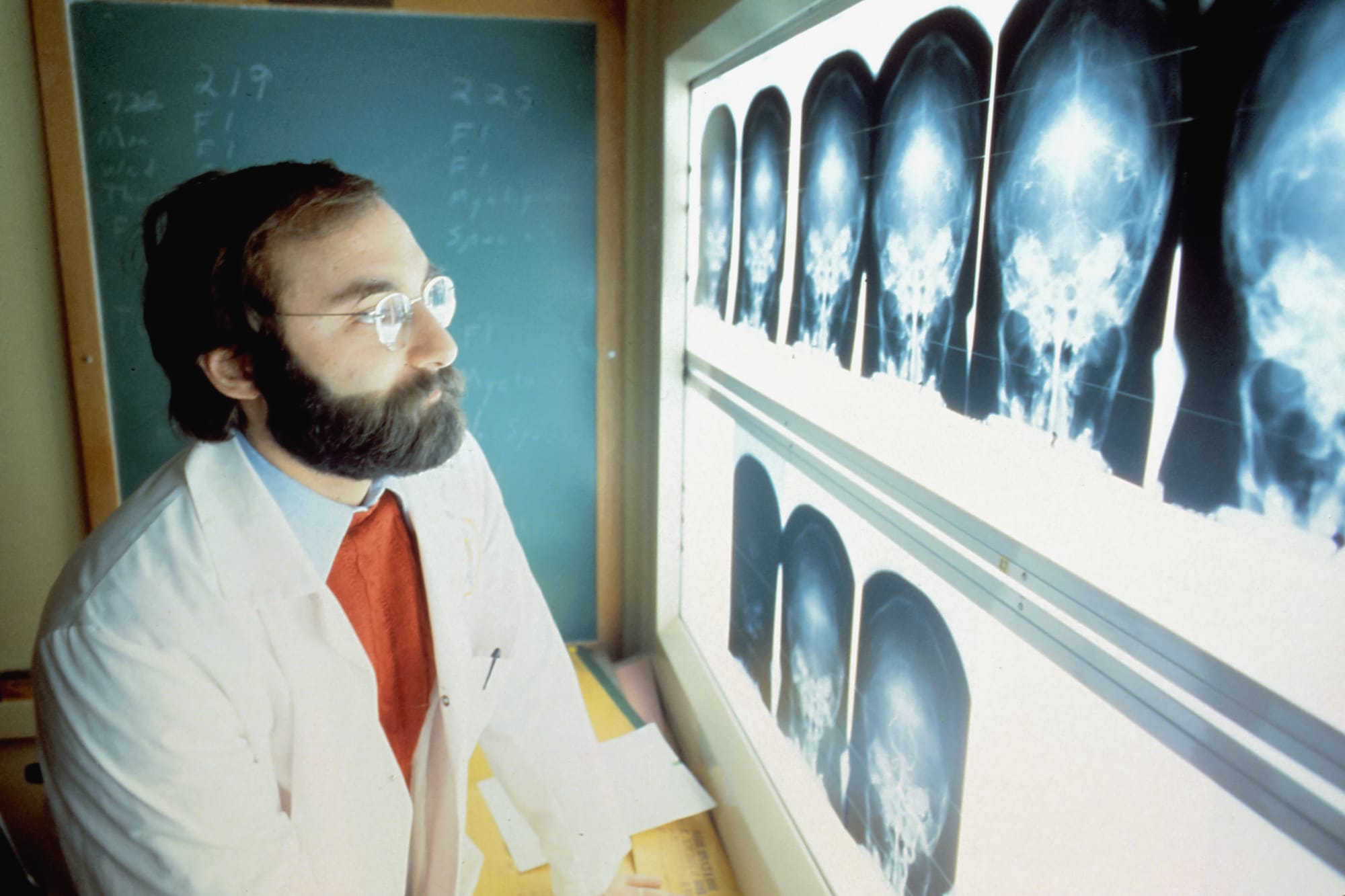
Generating synthetic health data requires custom algorithms and computing power, which can be expensive and time-consuming. Synthetic data can preserve some statistical properties of original data, but its accuracy and reliability depend on the quality of training data used to develop AI models in radiology or cancer research.
Despite these challenges, synthetic genomics holds tremendous potential for medical research beyond pathway and gene engineering. It can create fake patient records and medical imaging for non-identifiable datasets, enabling researchers to investigate new fraudulent situations while maintaining privacy.
Thus, synthetic data has advantages and limitations for use as training data in machine learning for medicine. Researchers should carefully consider these limitations when using synthetic health datasets to improve its accuracy and usefulness in clinical settings. While there are challenges involved in working with it, properly validated artificial datasets should lead the way forward towards innovation even more so at times where protecting personal privacy is at stake.
Case Studies Of The Negative Consequences Of Using Synthetic Data In The Medical Sector
Synthetic data has become a popular tool in the medical sector for analyzing patient information and developing new treatments. However, there are several negative consequences associated with its use.
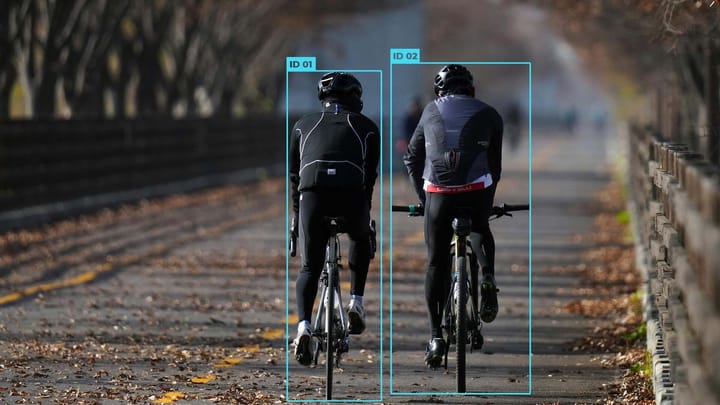
One major issue is the lack of diversity in synthetic data sets. Synthetic data is often generated from a limited sample size, which can result in biased algorithms that do not accurately reflect the diversity of real-world patients. This can lead to misdiagnosis and ineffective treatment for certain communities, particularly people of color who are already marginalized in healthcare.
Another concern is privacy and security. While synthetic data is designed to protect patient privacy by generating simulated datasets that anonymize individual patients' information, these artificial datasets can still be hacked or accessed by unauthorized users, putting patient confidentiality at risk.
Furthermore, relying on synthetic data can restrict innovation and creativity necessary for advancing medical research. Researchers may rely too heavily on pre-existing datasets instead of exploring new avenues of research or incorporating critical but hard-to-replicate real-world situations into their studies.
It is important to consider the negative consequences associated with using synthetic data in the medical sector before fully embracing it as a solution to improving healthcare systems. The issues concerning bias, privacy and security, and stunted innovation must be addressed through increased transparency surrounding parameters used to create synthetic datasets along with more comprehensive regulations surrounding their use while ensuring equitable representation across all demographics when creating such datasets.
The Importance Of Data Collection And Human Data Validation In Medical Sector
Data collection and validation are crucial in the medical sector to ensure the integrity and accuracy of medical data. With the rise of big data in healthcare, there are concerns regarding personal information and ethical issues that need to be addressed. Therefore, it is important to ensure that data is collected and managed securely.
The use of electronic medical/health records is becoming more prevalent, allowing for digital storage and maintenance of patient data. These records make it easier for healthcare professionals to access relevant information when providing care. However, with the vast amounts of data collected, proper validation is necessary to avoid spurious results.
Data standards play an important role in ensuring interoperability between computerized systems and applications, allowing seamless sharing of data. Medical big data are often difficult to access due to privacy regulations but enabling standards can ease this issue.
Overall, collecting and validating high-quality human health data is essential for decision-making by healthcare providers as it provides more accurate diagnoses, better disease management strategies along with drug discovery/treatment development among others including AI model training where synthetic or traditional dataset plays a vital role being input data source. The focus should be on ensuring processes that guarantee correct outcomes while complying with legal requirements surrounding safeguarding personal information invested within both collected biological samples at any clinical trials either from public or private databases which also pose serious safety concerns. In case of some systematic bias towards some categories improving accessibility while preserving privacy posture required by law frameworks.
Conclusion
While synthetic data has the potential to revolutionize medical research, it is important to consider the ethical implications and limitations of this technology. The use of synthetic data in medical research raises concerns around patient privacy and the accuracy of the data being used.
Additionally, case studies have shown the negative consequences of relying solely on synthetic data, such as misdiagnosis and inaccurate treatment plans. Therefore, it is crucial to prioritize data collection and human data validation in the medical sector. While synthetic data can be a valuable tool, it should be used in conjunction with traditional data collection methods to ensure the best possible outcomes for patients.


Comments ()